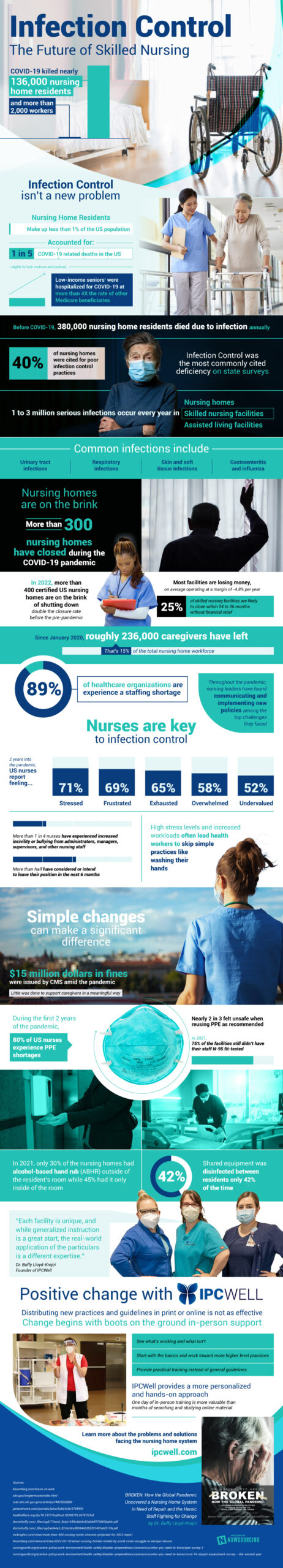
Infection control in healthcare settings is essential. It’s no secret that nursing homes felt the brunt of the damage during the pandemic. The coronavirus killed over 135,000 nursing home residents and over 2,000 workers. Although nursing home residents make up less than 1% of the population in the United States, they accounted for 20% of the COVID-19-related deaths. Older populations did not equally share the effects of COVID-19. Economic disparities were present in those who were greatly affected by the disease; low-income seniors were hospitalized for COVID-19 at over four times the rate of other Medicare beneficiaries.
Q2 2022 hedge fund letters, conferences and more
Infection control isn’t a new problem in the nursing home system. Before the pandemic occurred, almost 400,000 nursing home residents would die due to infection annually. Common infections like respiratory infections, urinary tract infections, gastroenteritis, and influenza were frequent in nursing home facilities. On state surveys, infection control was the most commonly cited deficiency; almost half of the nursing homes were cited for subpar infection control practices.
Nursing Homes Are Struggling With Infection Control And Financial Strain
Not only are nursing homes struggling with infection control, but they are also experiencing financial strain. Nursing homes are on the brink; over 300 nursing homes have closed during the COVID-19 pandemic. Following that, in 2022, more than 400 certified U.S. nursing homes are on the verge of shutting down. The closure rate in 2022 is double the rate pre-pandemic. Most facilities are losing money, operating at a margin of -4/8% each year. If this trend continues and nursing homes continue to operate without financial relief, 25% of skilled nursing facilities will likely close within the next 2-3 years.
The financial strain is also impacting nurses. Since January 2020, roughly 236,000 caregivers have left the field. Almost 90% of healthcare organizations are experiencing a staffing shortage because of this loss. The pandemic has left nurses feeling frustrated, stressed, exhausted, overwhelmed, and undervalued. Over one-quarter of nurses have experienced greater hostility from administrators, managers, and other nursing staff in the past two years. This negative work environment has impacted the way nurses can work. Higher levels of stress and increased workloads due to staffing shortages often lead health workers to skip simple practices like washing their hands.
Simple changes through infection control can make a significant difference. During the first two years of the pandemic, the majority of nurses in the United States experienced personal protective equipment shortages. While $15 million in fines were issued by CMS amid the pandemic, little was done to support caregivers in a meaningful way. New practices and guidelines tailored to a specific care facility is one of the best ways to enact change. A trained professional can see what’s working and what isn’t in the facility and provide practical training instead of general guidelines. Changes through in-person support are the best way to manage the issues plaguing the nursing home system.
Source: IPCWell.com